ALSO IN THIS ISSUE
The eye - a diagnostic window into memory and cognition
Is cancer overdiagnosed in younger people?
Diabetes dx and management still suboptimal globally
The eye - a diagnostic window into memory and cognition
The eye is a unique diagnostic resource that is underutilized in the diagnosis of neurological disorders. The retina, which translates light into the images we perceive, is the only part of the brain that can be directly viewed non-invasively, and eye movement is a “biometer” of conscious state. So, it is not surprising that research continues to demonstrate that analysis of the eye and its movements can be used for more than just diagnosing disorders of the eye itself.
Two recent papers continue this trend. One shows that patterns of eye movement in response to a recall question can detect memory deficits without the subject having to say a word - potentially very useful for young children and adults with speaking difficulties. (The obvious application to lie detection is not discussed.) The other demonstrates that applying AI to standard retinal images can identify those at higher risk of cognitive decline. Individuals with higher retinal biological age were up to 25-40% higher risk of developing cognitive decline or dementia over a five-year period.
COMMENTARY: More people go to the optician than to the neurologist, and retinal imaging is a routine part of optical care, making this second application particularly noteworthy. A side note - that paper is yet another using the large and comprehensive UK Biobank, which has become an enormously valuable resource for investigation of a wide range of disorders (it has limitations, particularly its bias toward the wealthy/white).
The light we cannot see - can diagnose cancer
Endoscopy is the mainstay of gastrointestinal (GI) cancer diagnosis. With that camera and light on the end of a tube, clinicians can check the lining of an esophagus, stomach, rectum, or intestine for signs of tumors. But the combination of a white light and a clinician’s eyes and brain has its limits. People miss stuff, especially when the signs are subtle.
However, there’s more to tumors than what can be seen by a human eye. To find it, researchers turned to hyperspectral imaging - the ultraviolet and near-infrared light just beyond the wavelengths that people can see. When they examined both healthy and cancerous animal tissue with this technique, they discovered that light reflected by diseased tissue has a different “spectral signature” from that of healthy tissue. And, critically, they were able to engineer a way to get those images through an endoscope, while still leaving enough room in the tube for clinicians to collect samples.
Is cancer overdiagnosed in younger people?
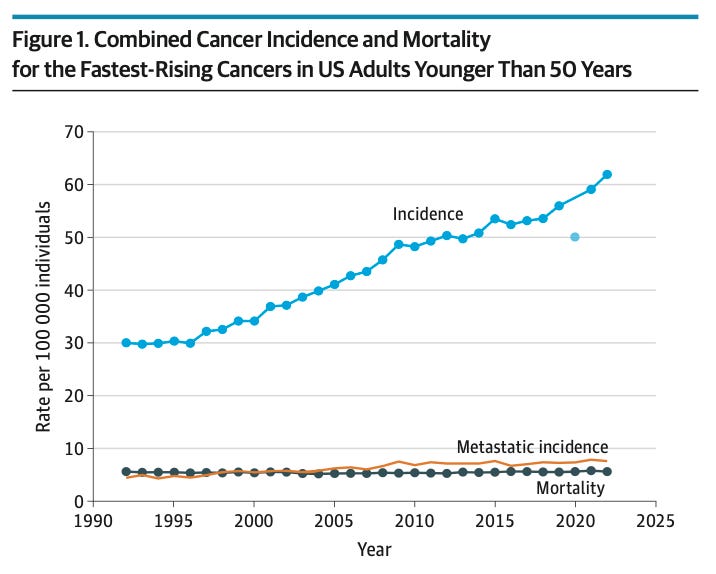
There is no question that cancer incidence in younger people has been rising. The trend is most notable for colorectal cancers, but it’s not exclusive to that flavor - for example, 4,800 more cases of early-onset breast cancer were recorded in the US in 2019 than would have occurred at 2010 incidence rates.
Why is this happening? A recent NYT article speculates that changing lifestyle factors (obesity, ultra-processed foods, etc.) and environmental exposures (toxins, microplastics, and more) might be to blame. One physician quoted in the piece claims that 40% of cancer cases could be avoided by lifestyle changes.
However, a recent paper in JAMA Internal Medicine asks whether the rise in early-onset cases is more a function of overdiagnosis than incidence. Vox has a very thoughtful review and reaction to the paper (paywall).
Overdiagnosis has a very specific definition: It’s the identification of disease that would not have led to significant symptoms or death. The paper’s primary argument is that although cases are up, deaths are flat to declining. The rate of death from cancer in those under 50 has decreased by nearly half since 1990. (Could that be happening because treatments are more successful? They say no.)
COMMENTARY: Overdiagnosis is concerning, because being its victim is far more life-changing than a false-positive result. (False positives can usually be resolved promptly.) In addition to anxiety, overdiagnosis can result in significant expense and time lost, not to mention side effects from treatment.
We need to remember that while cancer incidence in younger people is rising, in absolute terms cancer is still far far rarer in this cohort than it is in older people. While identifying cancers earlier typically permits more successful treatment, that reality must be balanced against another truth: Since the prevalence of the condition is low in younger people, the number of false positives will inevitably be high. Cancer-screening tests in this population will thus have low positive predictive value (the likelihood that a positive test is correct). Added to which are the true positives that would never have caused symptoms or death and would have been better ignored.
Multi-cancer tests are likely to increase diagnosis. That’s especially true for asymptomatic individuals with no suspicious history or other risk factors. It is for this reason that these tests are in trials in the UK and US to see what, if any, mortality benefit they can deliver. This paper’s evidence implies that real benefits are unlikely, at least at the population level.
Diabetes dx and management still suboptimal globally
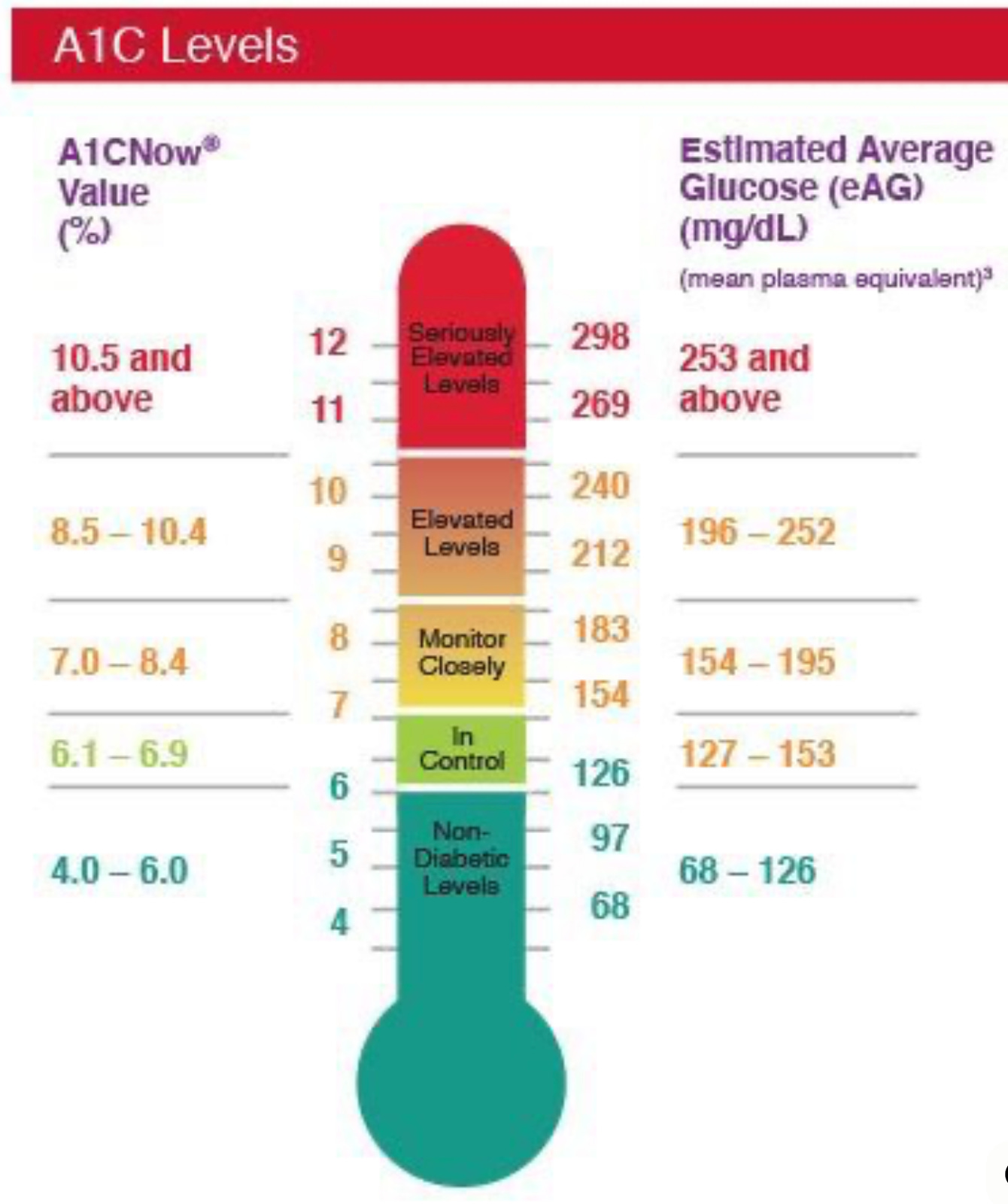
According to a recent report from The Lancet, 44% of people with diabetes worldwide remain undiagnosed. Once diagnosed, 91% of those do receive treatment, but only 42% of those manage to achieve healthy blood-sugar levels.
COMMENTARY: Uncontrolled diabetes drives serious damage to the eyes, the kidneys, the brain, and more, and there is growing evidence that this damage is dose-dependent. Even levels at the high end of the normal range cause a slow build-up of irreversible damage. HbA1c is the test of choice, since it reflects average blood-sugar levels over the past two to three months. Better diagnosis and management of this condition is urgently needed.
As next-generation sequencing (NGS) tests are being used well beyond oncologist offices, it’s critical that clinicians understand how to interpret their results and communicate about them with patients. To that end, the Association of Molecular Pathology just announced new recommendations for a standard template for reporting NGS test results.
Measles
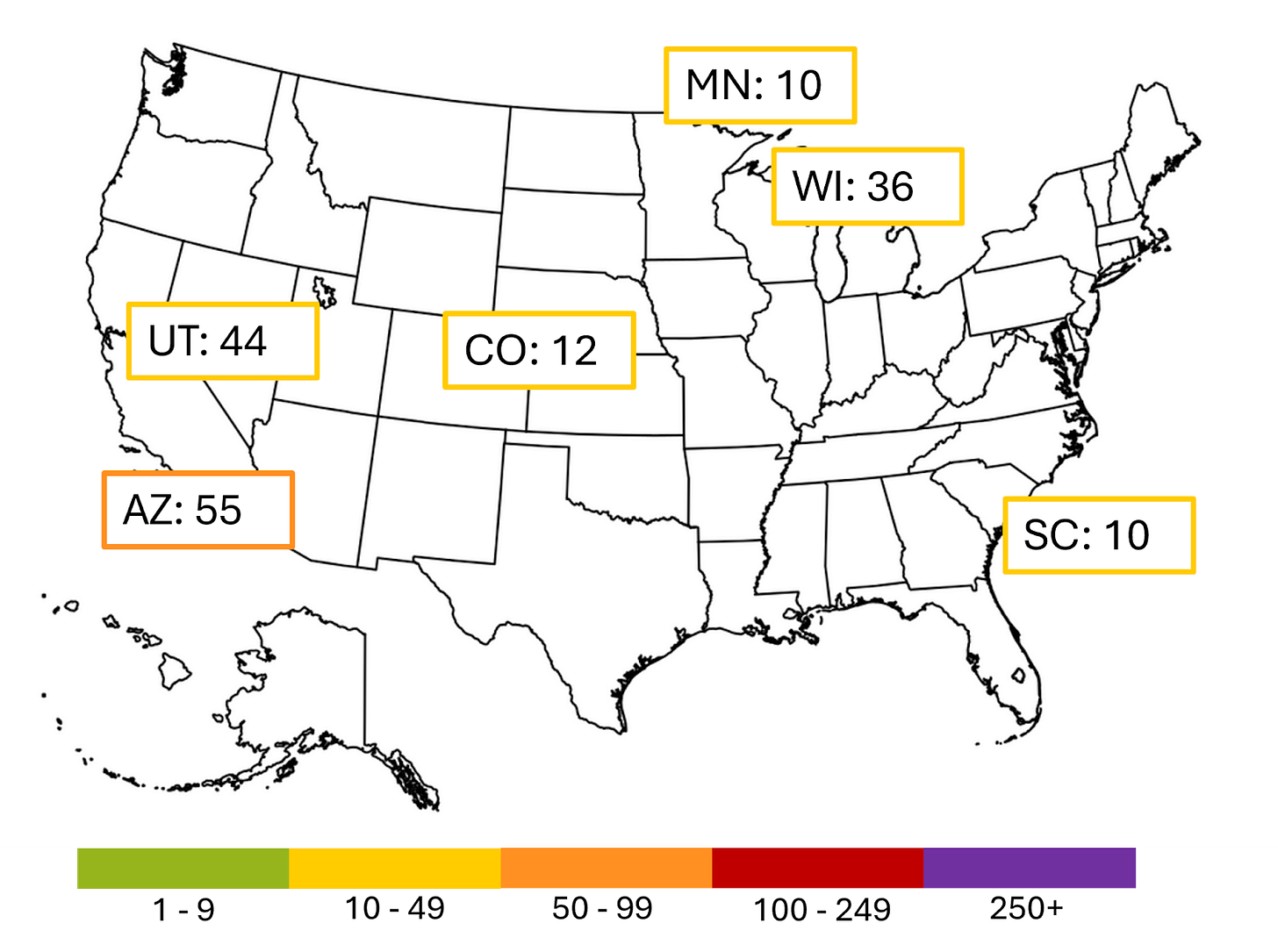
With the end of the outbreaks in New Mexico and Oklahoma, all cases linked to the large West Texas outbreak have resolved.
The current larger outbreaks in the US are shown below: Arizona, Colorado, Minnesota, Utah, Wisconsin, South Carolina.
Next week we will be attending the Arizona State University College of Health Solutions’ annual National Diagnostics Summit. But fear not! Sensitive and Specific will still appear in your inbox, with an issue focusing on Alzheimer’s Disease. Feel free to view the agenda and register to participate. Registration is free for all.