Pros and cons of newborn genomic screening
Volume 11, Issue 2 | January 9, 2025
ALSO IN THIS ISSUE
FDA updates pulse-oximeter guidelines
Bird Flu update
Patients read test results first. Write results with them in mind.
New pulse-ox guidelines aim for devices that work for everyone
We can’t say it any better than the STAT News January 6 headline on the subject: “FDA releases long-awaited guidance to improve accuracy of pulse oximeters for all skin tones.” Long-awaited as in decades. We’ve known for that long that these devices don’t work as well on folks with darker skin tones as they do on folks with lighter-colored skin. The big changes:
Lots more data required (3K data points instead of 200; suggested sample size at least 150 instead of the previous 10)
Per STAT News: “at least 25% of subjects should be in each of three groups: those with light, medium, and dark skin tones,” and in the third group, half of subjects must have very dark skin
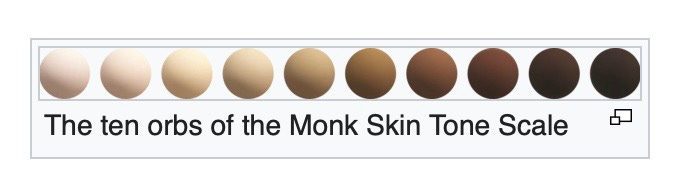
Skin tones are to be determined based on the Monk Skin Tone scale and the individual typology angle, which is based on spectrophotometry)
These are just draft guidelines, and don’t have enforcement teeth behind them. But manufacturers who follow them and get results showing that their devices worked properly get a marketing boost. They’re encouraged to place a “prominent statement” that “this pulse oximeter has been evaluated to perform comparably across groups of individuals with a wide variety of skin tones.”
Bird Flu Update
First bird-flu death in US
HHS announces $306 million more funding for H5N1 response
Virus strain in dairy cows may cause less-severe human disease
The patient hospitalized with H5N1 in Louisiana has died. They were infected as a result of contact with sick birds in a backyard flock and do not appear to have transmitted the virus to any other people. The patient was over 65 and had underlying medical issues. For a great overview of where we are now in terms of H5N1’s risk to people and what we can do about it, read this update from Your Local Epidemiologist.
The US Department of Health and Human Services has awarded an additional $306 million in funding for H5N1 response. The amount includes $103 million “for increased monitoring of individuals exposed to infected animals, testing, and outreach to high-risk populations (such as livestock workers)” and “$8 million to manufacture, store, and distribute additional influenza diagnostic test kits” for surveillance purposes.
The two recent severe cases of bird flu in humans were both caused by contact with birds, and that may not be a coincidence. New research indicates that the strain of H5N1 circulating in dairy cattle is likely to cause less-severe disease than a strain that circulated in wild birds in the past.
Since patients read test results first, write results they understand
In 2021, the 21st Century Cures Act required that all medical test results be posted immediately to online portals. Patients like having this access (evidence here and here). But the fact that so many people read their own results before their clinicians do has had the medical field wringing its hands. What about the increased worry that a small percentage of folks (8% overall, 17% of those with abnormal results, per one of the studies above) have when they see their results first?
A research letter in JAMA offers what we can’t help but think is an obvious solution: Write test results so that patients can understand them. Subjects were asked to read fictional prostate biopsy results. Some received reports written in a “university” style, others received reports in the style used by VA hospitals, and a third group received a patient-centered pathology report (PCPR).
Only 39% of those who read the university reports could tell that the report showed the presence of cancer. For folks who got the VA report, 56% figured it out. Ninety-three percent of the people who got the PCPR understood the message. And what’s more, participants’ level of worry was more closely associated with their risk level (i.e., high worry with high risk, low worry with low risk) if they read a PCPR rather than the standard reports.
More on the importance of diagnostic results that are easy for patients to understand to come in the 2024 Diagnostics Year in Review.
Parents like whole-genome newborn screening, is it worth it?
Newborn screening has been around for more than 60 years and has saved or improved countless lives. Today, all states require a blood-spot sample that is used to test for at least 29 conditions (most states test for a lot more than that - find yours here). So if blood-spot tests are good, would sequencing newborns’ entire genomes be better?
In early 2023, we published an in-depth review of this question. And as the cost of sequencing a genome continues to decline, the need to answer it becomes ever more pressing. Exploration into whole-genome newborn sequencing continues, with 11 different programs reporting from around the world.
One of these is the GUARDIAN trial (Genomic Uniform-screening Against Rare Diseases in All Newborns), a project of the New York State Newborn Screening program. A recent JAMA report presented interim findings on the first 3,982 newborns of a planned 100,000 the trial intends to enroll. Whole genomes were sequenced, with 237 genes analyzed in detail. Some highlights:
A strong majority of parents wanted to participate: 72% signed up. The most common reasons for not participating were lack of interest (31% of respondents), feeling that standard screening was enough (21%), and being overwhelmed by having just had a baby (14%).
Relatively few diagnoses were reported that would not have been picked up by standard screening. The most common one was G6PD deficiency (92 newborns; this is an X-linked disorder primarily affecting boys, managed by trigger avoidance). Seven babies had a GJB2 deficiency resulting in hearing loss, of which only two would have been detected by standard screening, and five had HBB deficiency, resulting in sickle-cell disease.
Of the newborns who were flagged as having concerning genetic variants, 19% were found on further investigation to be false positives. All of the cystic fibrosis diagnoses (11) turned out to be false, although it is possible that milder symptoms might develop in some of these newborns in later life. [UPDATE: See addendum below]
COMMENTARY: This research does not make a strong argument for whole-genome screening of all newborns, especially considering the false-positive rate. We will learn more as the trials continue. The arguments for a “yes” answer are strong when it comes to disorders that arise in childhood. But for disorders that don’t appear until adulthood or even later (e.g., Alzheimer’s), the decision is more complicated.
ADDENDUM, January 17, 2025
One of the study’s authors drew our attention to the fact that the 11 cystic-fibrosis diagnoses noted above were based on the presence of two genetic variants that are not well correlated with cystic fibrosis disease. (In other words, just because a baby has those variants doesn’t mean they’ll get sick.) If those 11 diagnoses are excluded - which they were after the first 1,000 subjects in the study - then the study’s false-positive rate decreases dramatically. Instead of a 19% false-positive rate for whole-genome newborn screening, the rate would be 9%.
Quick Hits
Many drugs used for cancer chemotherapy can hurt the kidneys. But it can take several days before the effects of that damage show up in a blood test. New research has identified six biomarkers in urine that can help clinicians detect kidney damage within 24 hours of injury. In addition to being used in the clinic, biomarkers could help researchers develop drugs that are safer for the kidneys.
How much protein or DNA does a test need to detect in order for it to turn positive? Researchers have built a nanopore-based circuit that can detect the presence of a single molecule. Biological samples are loaded into the device along with salts, which break up into ions that can flow through the nanopore. If a protein or DNA molecule from the sample passes through the pore, that reduces the flow of ions, triggering the detector.
COVID & COVID/Respiratory EUA Update
The FDA issued three new COVID 510(k) premarket notifications, no new EUAs, no amendments to existing EUAs, no revocations and no warning letters in November.
510(k) Premarket Notifications: 3 [Nuclein, LLCDASH SARS-CoV-2 & Flu A/B Test | Abbott Alinity m SARS-CoV-2 AMP Kit | Abbott Alinity m SARS-CoV-2 CTRL Kit]
New EUAs: 0
Amendments to Existing EUAs: 0
Revocations/ Warning Letters: 0