In This Issue
COVIDtests.gov reopens
New AI use case: Create a better Dx for your Tx
New AI diagnostic trains itself successfully
Should mammograms start at 40?
New and Noteworthy
Free at-home COVID tests available again
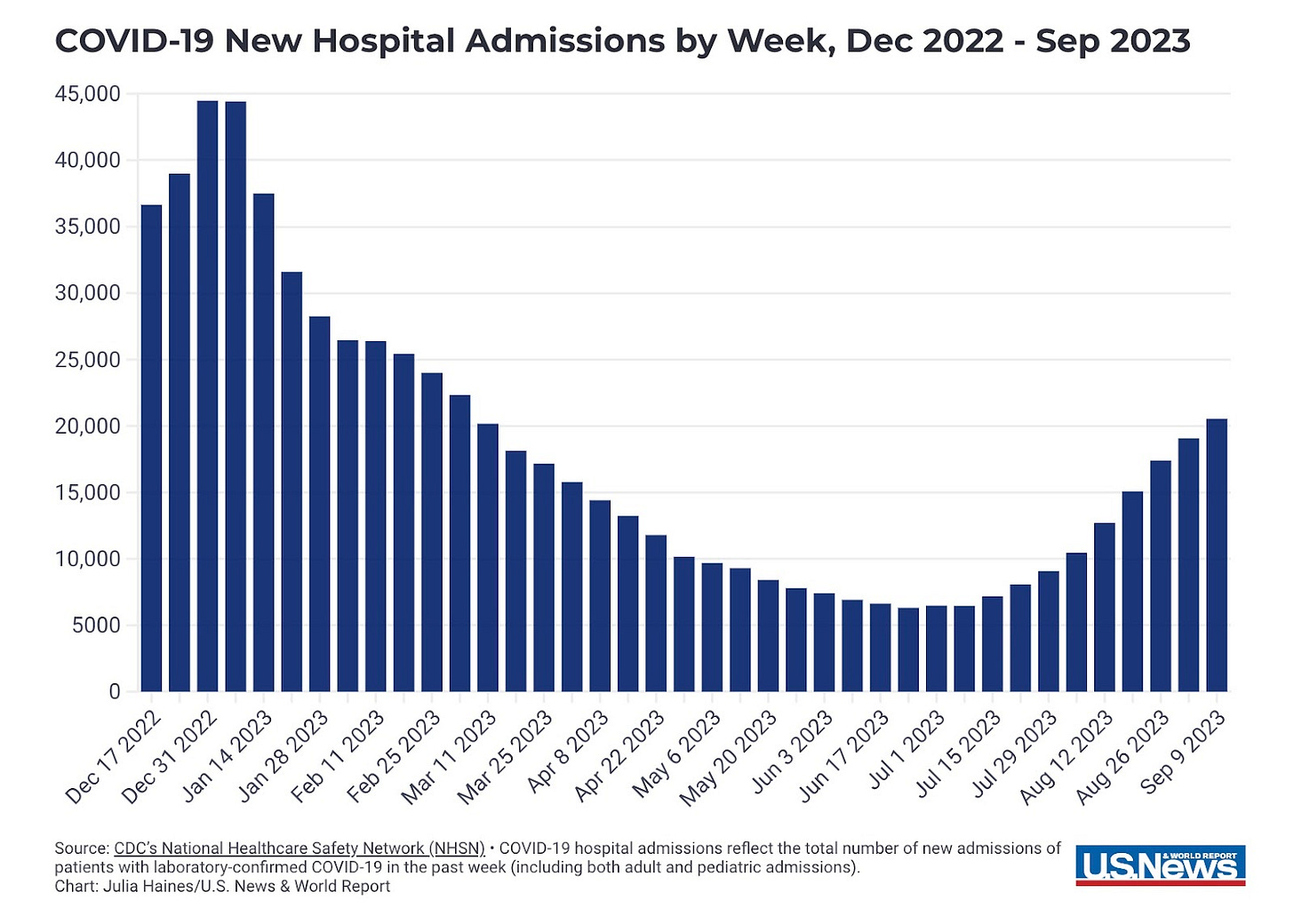
Given the current surge in infections as well as 10 straight weeks of increased hospitalizations, the Biden administration just announced that COVIDtests.gov will reopen on Monday, September 25. When that happens, each American household can once again order four free COVID tests. There are 12 companies involved, for a total of 200,000 tests. Making tests for free is aimed at encouraging proactive use of home testing and isolation as needed.
Commentary: We will stick with our mantra, “Testing is the only way to slow a surge.” We applaud the administration for their action here - we hope that uptake is broad and rapid. But just because you can get new tests, don’t throw away your old ones - including those that appear expired. Check the FDA website to see if your old tests are still good to use. Note: Mara is on the board of OraSure, one of the 12 companies that will be supplying tests.
New AI use case: Find the patients who need your drug
Another week, another new use for AI. This week’s first new use case: When you have a drug for a condition, but you want a better way to screen for it, so that more people will be diagnosed with the condition and thus buy the drug.
Bristol Myers Squibb (BMS) has the drug. It’s Camzyos, used to treat hypertrophic cardiomyopathy (HCM), a condition in which the heart muscle becomes pathologically thickened and cannot move blood properly. The AI-based screening tool is Viz HCM, which, as STAT News reported, “looks at 12-lead electrocardiograms collected during routine care and flags suspected cases of . . . HCM for further evaluation.” It was developed by Viz.ai with support from BMS, and received FDA approval in August.
Of note: As of October 2022, the FDA had approved 521 AI-based algorithms, of which nearly 400 involve radiology. We certainly expect many more to come in widely diverse areas. The Medical Futurist has summarized these tests and their impact.
Why train AI to diagnose pathology when it can train itself?
Okay, so we got your attention with a bit of an alarmist, “We welcome our new robot overlords” headline. But seriously, folks in the UK did just publish a paper in Nature explaining how their new AI model, RETFound, trained itself to diagnose pathology based on retinal images. The big breakthrough here, diagnostics-wise, is the ability to develop AI-based diagnostics more easily, with less human work involved.
The method of training in question is called “self-supervised learning.” It was made famous by your old friend ChatGPT, which uses tons and tons of text written by humans to understand what writing in English is supposed to look like. RETFound was trained in a similar way, using 1.6 million unlabeled images of retinas to learn what a retina is supposed to look like.
Once it had done that on its own, the researchers gave RETFound just a small sample of labeled images showing the difference between healthy and diseased eyes with various conditions, both ocular (eg., glaucoma, diabetic retinopathy) and systemic (eg., heart failure, Parkinson’s disease).
In all cases, RETFound performed better than other, human-trained AI models had done, and it did particularly well at diagnosing ocular disease. As a Nature news article reported: “On a scale where 0.5 represents a model that performs no better than a random prediction and 1 represents a perfect model that makes an accurate prediction each time, it scored between 0.822 and 0.943 for diabetic retinopathy, depending on the data set used.”
To screen for prostate cancer, look to MRI, not PSA
A digital-rectal (DRE) procedure combined with a prostate-specific antigen (PSA) test has long been the standard of care for prostate cancer screening (see the USPSTF recommendation here). But for much of the last decade, there have been serious concerns about PSA’s low sensitivity (missed cases/false negative rate) and specificity (unnecessary biopsies/false positive rate). A 10-year UK study published in 2018 showed no difference in cancer death rate with or without PSA screening.
Enter MRI. In 2018, the Swedish national guidelines on prostate cancer started recommending that men undergo prostate MRI before biopsy. A recent Swedish study compared outcomes for men in one Swedish region during the years just before and after that change was made. The result: Adding MRI meant 16% fewer were biopsies performed, with a 30% reduction in negative biopsies (aka PSA false positives).
A UK study came at the problem from the other direction - what happens when MRI is used alone as a screening test? Irregularities (lesions) were found in 21% of MRIs, of which 52% were confirmed on biopsy. Perhaps most telling, 60% of these confirmed cases had PSA <3ng/ml (aka PSA false negatives).
Bottom line: Both recent studies confirm that a Dx pipeline of MRI for those with a PSA >3ng before biopsy is far superior to moving directly from high PSA to biopsy.
Food for Thought
Is extending mammography down to age 40 worth it?
Screening always sounds like a good idea. Who wouldn’t want to know that they have a disease that, if identified, could be treated successfully? However, screening has two inherent challenges:
Finding a test/analyte that best matches the pathology is hard, especially if we don’t really understand the driving pathology (see PSA below).
Screening is designed to find cases that are, by definition, not easily noticed. This often means testing a large group of people for a disease that only a few will have. And since no real-world test can be perfect, the rarer the disease you’re testing for, the greater the number of false positives, even for a great test.
This week NEJM published a perspective arguing against the US Preventative Task Force’s (USPSTF) proposal (not yet agreed) to extend routine screening from women over 50 years to women over 40 years. While extending biennial mammography to this group over a decade is estimated to reduce the death rate from 0.31% to 0.23% (that’s one extra life per 1,000 tested), it would likely come at the cost of 36% false positives, one fifth of which would be biopsied unnecessarily.
Quick Hits
Wisconsin researchers showed that wastewater levels for flu and RSV there increased one to two weeks before emergency-department visits for those viruses went up.
The University of Texas at San Antonio and the UT Health San Antonio Long School of Medicine have partnered to create what they say is the first of its kind: a five-year combined doctor of medicine / master of science in artificial intelligence degree program.