In This Issue
COVID diagnosis by wearable devices
Using dogs to detect COVID
State of the pandemic in three news articles
AI for infectious-disease surveillance vs. clinical use
New and Noteworthy
Your watch says it might be COVID time
What if your watch could tell you if you have COVID? The US Department of Defense, in partnership with Philips, has been working on a device-agnostic algorithm that uses biometric data from off-the-shelf wearable devices to diagnose the disease. The military has been field-testing it at least since 2021, and published results about it in Nature Scientific Reports in 2022. According to DOD, the algorithm can diagnose cases of COVID and other infectious diseases up to 48 hours before symptoms show up, and has given early warnings of the possibility of illness “up to six days prior to onset.”
For now, the tool only works on a couple of brands of devices and is only available to certain military service members. But Philips is now offering the algorithm under a licensing model. We’ll be interested to see if, when, and where it gets picked up.
Dogs’ noses pass the COVID sniff test
A study in California schools looked at the ability of trained sniffer dogs to detect COVID infections in people, using the results of concurrent antigen tests to determine whether the dogs got it right or not. According to that metric, over the course of about 4,000 screenings, the dogs had a sensitivity of 83% (95% CI 75-90) and a specificity of 90% (95% CI 89-91).
Commentary: Did you spot the “catch” in this article? All due respect to antigen tests (we still love them), but we know their sensitivity isn’t perfect, especially in the earliest stages of illness. Dogs’ noses, by contrast, have time and again showed that they can be more sensitive than the best available lab tests for detecting illness including cancer.. We would have loved to have seen the dogs go up against both antigen and PCR. We’d be willing to bet that some of the dogs’ “false positives” were true positives - that the antigen tests were the ones who got it wrong.
COVID: Where are we now?
Wondering about the status of the pandemic and our response to it these days? Three news stories that showed up this week tell you everything you need to know:
From the Washington Post: Last week, the CDC held its first in-person annual conference in four years, with no COVID precautions in place. As of now at least 35 people who attended the conference have tested positive for COVID.
From the Boston Globe, on May 2: For the first time since the pandemic began, Tufts Medical Center in Boston had no inpatients with COVID. Another hospital, Boston Medical Center, also logged zero COVID inpatients as of last Thursday.
And from the Atlantic’s article, “Will COVID’s spring lull last?”: “This might be the longest stretch of quasi-normalcy that humanity has had since 2020’s start, but experts can’t yet tell whether we’re at the beginning of post-pandemic stability or in the middle of a temporary reprieve.”
Commentary: To sum up: For now, COVID isn’t killing nearly as many people as it has in the past. (Although COVID still creates 80,00+ new reported cases - likely 5x that in reality - with 1,000+ deaths each week). Clearly, it sure as heck isn’t gone, so if we bring large groups of people together without any precautions, some of them are going to get infected. The question is, are we worried enough to do anything about it?
Food for Thought
You’ve learned to swab your nose. How about drawing some blood?
True self-testing has four steps:
User decides to test
User collects sample outside of a health-care facility
User carries out the test process
User receives the test’s results, interprets (and hopefully acts on) the results there and then, far more quickly and cheaply than they would have been able to do with a lab-based test.
The more difficult, complex, or subtle any of these steps is, the less practical a self-test is. Adequate and accurate sample collection for some analytes is the major hurdle. (Spinal CSF draw or prostate biopsy, anyone?) The increasingly successful assault on this challenge uses newer, more sensitive equipment to find smaller and smaller quantities of target analytes present in less invasive samples such as swabs, finger sticks, saliva, urine, sweat, or breath. For more invasive samples, the solution is more complex.
Blood and serum collection, in particular, have been an ongoing challenge. The gold standard for blood and serum sampling is a phlebotomist, in a lab or a doctor’s office, collecting 5 - 10 ml of venous blood in a set of tubes, each with a different stabilizer/preservative. Capillary blood (blood not taken from veins or arteries) as a sample has also been the subject of considerable innovation of late. While it is unlikely to be as reliable as venous blood for broad panels, and there are other tests for which it simply can’t be used, capillary blood is perfectly adequate for certain diagnoses.
One new sampling technique allows a person to take their own capillary blood sample at home. And we don’t mean just a finger prick, but a sample large enough to be sent to a lab for analysis. The devices differ by company, but generally consist of a disk with one or more tiny needles, which is placed on the patient’s upper arm or thigh. Over a period of 30 minutes or more, these micro-needles sip capillary blood and deposit it in the disk. At the end of the process the disk is removed, sealing itself upon removal and is sent to a lab for analysis.
Commentary: While relatively new, we expect these home blood collection devices to gain in popularity. First use will likely be in cancer patients undergoing treatment who need regular monitoring of their blood chemistry.
AI to diagnose disease: Surveillance vs. clinical medicine
This week NEJM published a review of how artificial intelligence may be increasingly used to improve infectious disease surveillance (see extracted Figure 1 for uses, methods, and references). Three weeks ago an NEJM companion review summarized the history of applications of AI in clinical medicine. Complex as it is, clinical diagnosis is both simpler and more immediately consequential than surveillance. In the clinic in which the patient is present, all the data available pertains to this patient, more tests can be ordered if needed, and success or failure are rapidly apparent. With surveillance, the available data is limited and unrepresentative (e.g., only 1,400 US wastewater sampling locations), non-specific (e.g., “flu-like” symptoms), and/or tangential (search requests for coughs). The consequences are greater - affecting entire communities - but outcomes are more indirect.
There has been increasing interest in using AI in medicine generally - NEJM has increased its coverage of the topic to support the 2024 launch of a new journal to be called “NEJM AI”. But what exactly is AI? At the most obvious level it is decision-making (the intelligence part) done by a computer (the artificial part).
The FDA, which regulates clinical devices, has struggled with deciding what constitutes AI, given that (almost) every device approved for use in the clinic provides at least some degree of decision “support,” using algorithms with varying degrees of complexity and requiring varying degrees of human intervention. The agency currently maintains a list of what it calls “Artificial Intelligence and Machine Learning (AI/ML)-Enabled Medical Devices” to which it has given approval, suggesting that the involvement of machine learning is what puts a device into AI territory as far as they’re concerned. The list includes 521 devices to date, of which 200 were in 2021-22 - but they note that other FDA-approved AI/ML-enabled devices may be out there that they don’t know about. The earliest of these devices were all forms of image analysis (X-ray, MRI, CT, ultrasound, etc.), followed closely by devices used in cardiology.
The FDA does not regulate surveillance tools, but the need for machine learning is much greater than in clinical applications simply because the available data is so much more diverse and indirect - an ML-based approach can seek out hidden patterns that enable it to spot the nature and location of emerging pathogens.
Commentary: The challenge is that the more the machine learns on its own, the more difficult it becomes to figure out how the conclusions were reached, especially during brief and urgent patient encounters. And we can’t forget that - for now - human beings, with all their potential biases, are still the ones who set up the machines and how and what they learn - at least initially.
Quick Hits
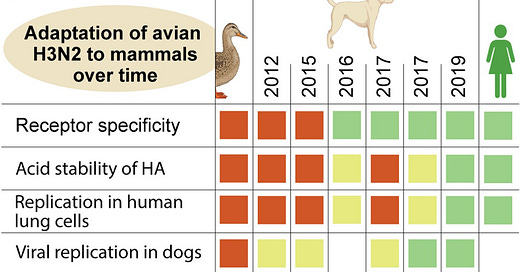
Flu edges closer to spilling from dogs into humans. All influenza comes initially from birds, then reaches us by prior infection of an intermediary species. Recently Chinese scientists sequenced influenza virus from 4,000 sick companion dogs over 7 years (pre-COVID) and found that canine H3N2 influenza is becoming closer and closer to variants known to infect humans.
EUA Update
The FDA issued one new 510(k) premarket notification, four new EUAs, 11 amendments to existing EUAs, and three revocations in April. Data is available at TestingCommons.com
510(k) Premarket Notifications (1): Biofire Spotfire Respiratory (R) Panel Mini
New EUAs (4):
Molecular (2): MedArbor Diagnostics SARS-CoV-2 Assay | University of Massachusetts ICTC SARS-CoV-2 RT-PCR Assay
Antigen (2): Azure Biotech Fastep COVID-19 Antigen Pen Home Test | Princeton Biomeditech Corp. Status COVID-19 Antigen Rapid Test for Home Use
Amendments to Existing EUA’s (11):
COVID Molecular: 5
COVID Antigen: 6