ALSO IN THIS ISSUE
Diagnosing preeclampsia early in pregnancy - finally
Good news about heart disease
ctDNA edges towards clinical use
CDC ends bird flu emergency
Highest annual measles cases in 33 years
A first-trimester blood test for preeclampsia
Preeclampsia, a high-blood-pressure syndrome of late pregnancy, can be deadly to both mother and fetus. But diagnosing it before it’s already happening has proved difficult. In research presented at the Annual Meeting of the European Society of Human Reproduction and Embryology, a blood test that uses cell-free RNA (cfRNA) as a biomarker was able to predict both the early- and late-onset versions of the condition. When used in the first trimester, it had 83% sensitivity and 90% specificity for early-onset preeclampsia and 86% sensitivity and 89% specificity for late-onset.
The researchers used machine learning to identify which cfDNA sequences indicated preeclampsia. They also discovered that the cfDNA that predicted the early-onset version were different from those predicting the late-onset version, indicating that the two conditions have different causes.
COMMENTARY: Microsoft’s AI diagnostics aren’t quite all that
At the end of June, the tech-nerd press got very excited about the Microsoft AI Diagnostic Orchestrator. An AI diagnostics platform that’s 4x better than human doctors at diagnosing complex diseases! Pretty soon we’re all gonna have tricorders, just like Dr. Crusher in Star Trek: TNG! (C’mon, if you’re a GenX nerd like Liz, you know you watched it, too.)
This week, STAT News injected a welcome dose of sanity to the discussion. Yes, Microsoft’s platform performed much better than doctors - under circumstances that don’t reflect what being a doctor is really like. The two big issues:
The platform was tested against super-complex cases that are rare in general practice. Most cases that doctors see are much more straightforward than these.
The doctors in the study were not allowed to look anything up or consult with anyone else, which is exactly what doctors do when faced with complex cases.
That being said, the AI platform might still be more accurate than humans - but the difference might not be so dramatic. STAT News pointed out that Google tested its diagnostics platform, the Articulate Medical Intelligence Explorer (AMIE), in much the same way as Microsoft did, using super-difficult medical cases. The result:
Google’s tool was able to get the right diagnosis in its top 10 list of possibilities 59% of the time, compared to 33% of the time for unaided physicians. Physicians aided with a search engine (44%) did better than unaided clinicians, but using AMIE for assistance increased their accuracy further (52%).
Bottom line: It may end up being true that for the hardest cases, doctors should simply listen to the AI. But it will be interesting to see what the tech does when faced with the humdrum day-to-day cases - and what it learns from them.
Two servings of good news about heart disease
First, per just-published analysis in the Journal of the American Heart Association, the number of heart attacks (aka myocardial infarction, or MI) in the US has dropped 90% in the last 50 years. How and why? For starters, smoking is way down, and the use of aspirin and statins is way up. In addition, heart-bypass surgery, arterial stents, and balloon angioplasty have been widely embraced. And for those who do have an MI, survival rate has increased from 60% to 90% during the same time, thanks to widespread availability and use of portable defibrillators.
The other good news comes in diagnostics for heart disease, specifically HCM. Each year, about 1% of adults with HCM will experience sudden cardiac death (SCD), an obviously dire situation that requires quick treatment with a defibrillator. (The rate in kids is even higher, at 6 - 8 %.) But it’s been nearly impossible for doctors to determine which patients are at high risk for these events. We do know that fibrosis of the heart muscle puts folks at high risk of SCD, but that’s been extremely hard to diagnose.
As usual of late, AI has come to the rescue. A new model described in Nature Cardiovascular Research is able to identify fibrotic tissue in MRIs of HCM patients’ hearts, something that humans have never been able to do. By combining that data with the patient’s medical record and other imaging history, it reached 89% accuracy in its predictions. The traditional clinical guidelines only have 50% accuracy, so this tool is another big step in the right direction for diagnosis and treatment of heart disease.
Bird Flu: CDC ends H5N1 emergency
The CDC ended its emergency response to bird flu last week. The change was made because there have been no reported human cases since February and cases in animals have decreased.
“This was not something that was imposed from the top down. It was initiated by the career scientists at CDC,” Dr. Nirav Shah, former CDC principal deputy director, told CNN. “If there were to be more human cases, it is very easy to ratchet back up the level of the intensity of the response. It can literally be done in an afternoon.” According to HHS, regular surveillance for all types of flu, including H5N1, will continue at non-emergency levels.
Measles:
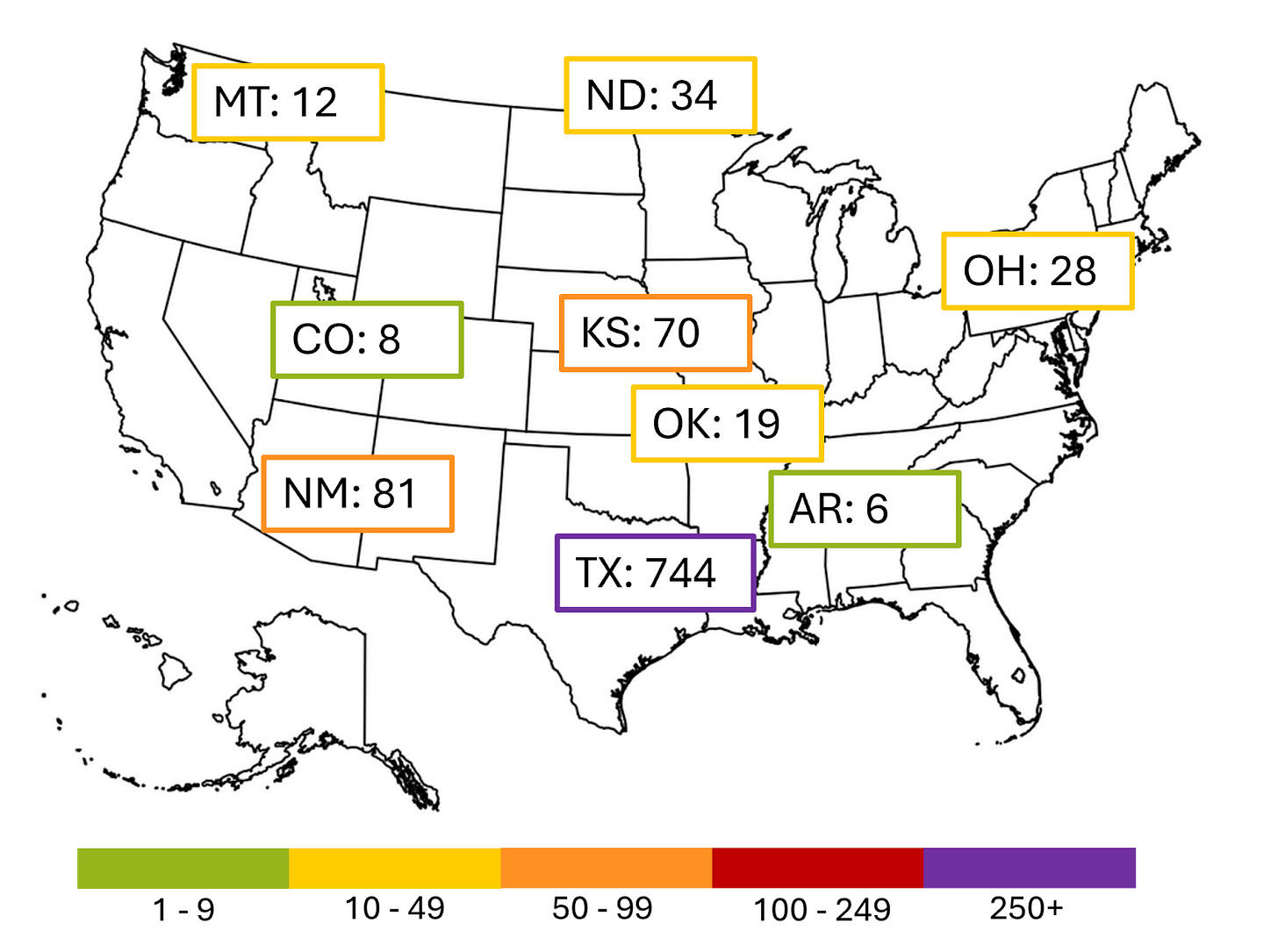
As of yesterday, the US has seen 1,288 cases of measles this year. That’s the highest number since 2000, the year that the disease was declared eliminated here and the largest number of cases since 1992. (That declaration is made by the WHO. It means that measles isn’t endemic here - outbreaks only happen when the disease is brought in from another country and then starts spreading.) The country will lose that status if an outbreak here lasts more than 12 months. The outbreak centered in West Texas is about halfway to that point, but fortunately it’s slowing down. Fingers crossed.
The current larger outbreaks are shown below. The cases in Texas, New Mexico, Kansas, and Oklahoma all came from the same source; those in Arkansas, Colorado, Montana, North Dakota, and Utah are unrelated.
Circulating tumor DNA edges toward clinical use
At American Society for Clinical Oncology meetings this spring, participants expressed both excitement and caution about the use of circulating tumor DNA (ctDNA) in the management of cancer.
The excitement came from ctDNA’s ability to improve management of cancer recurrence after initial treatment. Since ctDNA appears in blood up to 18 months before imaging can detect recurrence, it offers an opportunity to identify resistance and change therapy to head off progression. The caution centered around the lack of evidence of reduced morbidity and mortality as a result. Several trials are underway that will - we hope - clarify this issue.
COMMENTARY: Understanding how tumor type and therapy management change the dynamics of ctDNA will take some time. But as a practical matter, cancer survivors should insist on these tests as part of their post-treatment observation and management strategy.