ALSO IN THIS ISSUE
Rapid TB test using saliva as sample
Could overuse of CT scans raise cancer rates?
Where might a polygenic risk score fit in prostate-cancer screening?
A no-contact skin monitor
Bird Flu Update: Pasteurization kills virus
Rapid point-of-care TB test can use saliva as sample
“A new smartphone-sized device can deliver tuberculosis (TB) test results at the point of care in less than an hour,” the Center for Infectious Disease Research and Policy reported. The test is the first to be able to detect TB in saliva as well as in blood or sputum (coughed-up gunk).
COMMENTARY: The device was created with low-resource areas in low- and middle-income nations in mind, as that is where 90% of new TB cases arise. But with public-health resources in the US in steep decline due to federal funding cuts and local legislation curbing the power of public-health officials, it could ultimately be of use here, as well. (Click for more info about the current large TB outbreak in Kansas.) TB is highly contagious, but it’s also highly treatable if diagnosed early.
Breath: The ultimate non-invasive triage tool for lung cancer?
Exhaled breath contains a rich and dynamic mix of many hundreds of organic compounds. Interest in finding biomarkers in this stew has grown steadily over the past 25 years, but early exploration failed to identify any that were able to drive a differential diagnosis (see this 2023 review for details).
That’s changing. Last month, Annals of Oncology published a study in which breath was used to diagnose lung cancer in patients who were suspected of having the disease. The system uses an “electronic nose”: two arrays of semiconductor sensors. The nose continuously compares the levels and mix of 30 compounds in inhaled room air versus those in exhaled breath. (This, by the way, explains the problems that earlier researchers had with breath. You need to measure a lot of compounds in it - using just one or even a few of them doesn’t work.)
Reported results are impressive. For patients with chronic obstructive pulmonary disease (COPD), positive predictive value (PPV, the likelihood that someone who tests positive does have the disease) was 79%, and negative predictive value (NPV, the likelihood that someone who tests negative doesn’t have the disease) was 89%. Among those without COPD, PPV was 71% and NPV 100%. Interestingly, the results did not vary by tumor characteristics – earlier, remote tumors were identified as reliably as later-stage metastatic disease.
COMMENTARY: If breath is to come into its own, this integration of low-cost sensors, cloud integration, and pattern matching by artificial intelligence must be the direction to explore.
On the cautionary side, this was a relatively small study in which all the patients included had respiratory problems so severe that lung cancer was already suspected. So while we should not plan on using this test to screen a more general population, it could be highly valuable in triaging patients into those meriting more invasive testing versus those for whom watchful waiting is reasonable.
Bird Flu Update: Pasteurization kills the virus
USDA adds funding for preparedness, detection, response research
Researchers have confirmed that pasteurization kills the H5N1 virus. Heating milk to slightly lower temperatures for longer (54 degrees Celsius for 10 minutes or more) will also do the trick. However, the team reported, active virus can persist in untreated milk for “as long as eight weeks at refrigeration temperatures.”
Last week, the USDA’s Animal and Plant Health Inspection Service “announced $15.3 million in funding for research projects to enhance preparedness, early detection, and rapid response to the diseases that threaten US livestock,” the Center for Infectious Disease Research and Policy reported. Roughly $5.1 million will go toward biosecurity, while about $1.4 million will go towards emergency-response planning.
Funding for the USDA’s five-pronged strategy for battling H5N1 (which we reported on last month) “will rely on money cut from programs meant to help schools and food banks support local farmers,” Politico reported today.
Measles Outbreaks: Third confirmed death; federal funding cuts hurt response
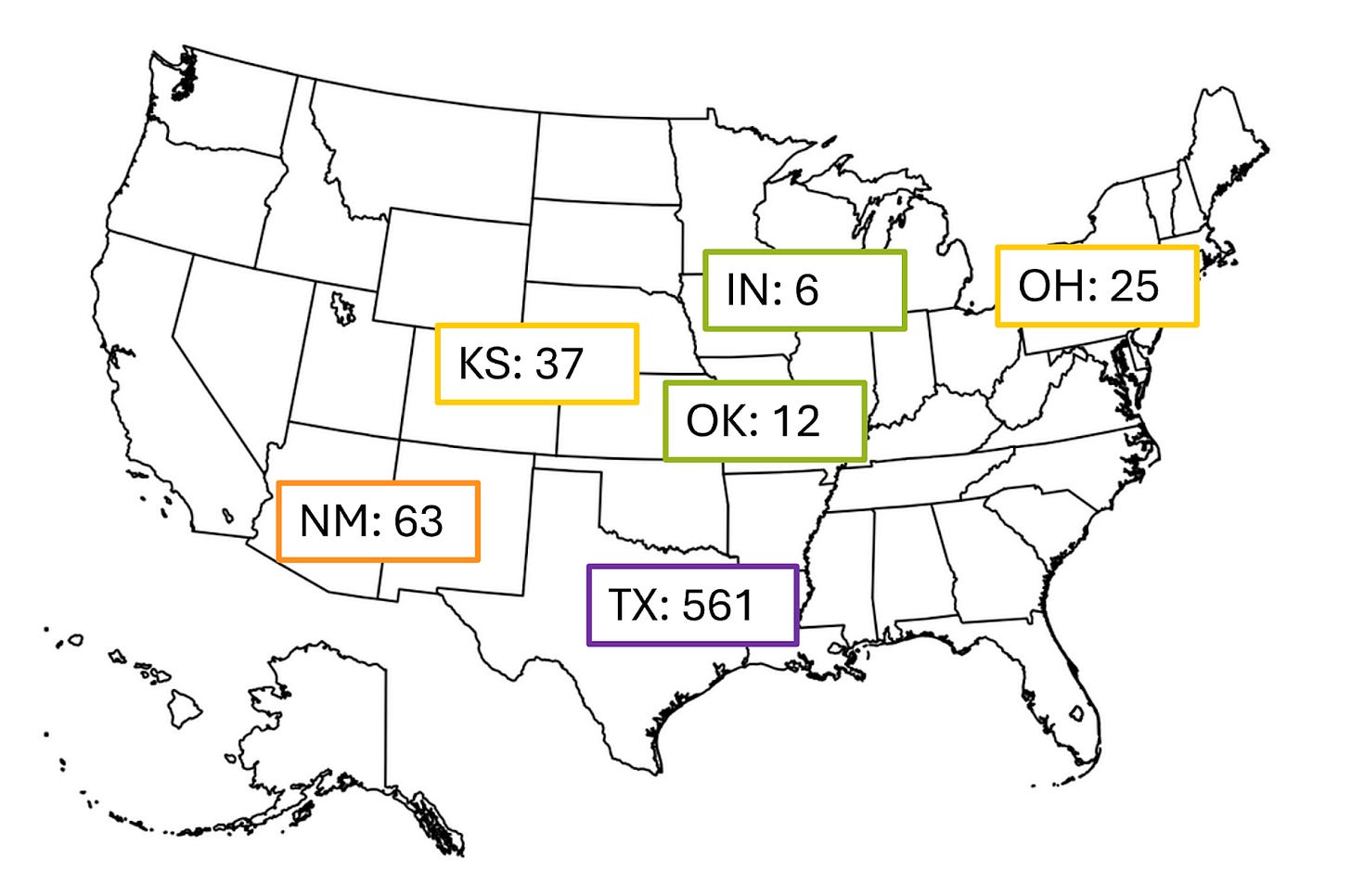
Last week, 105 measles cases were reported in the US. It’s the first time since a large 2019 wave that the weekly number of measles reports in this country was over 90. Unfortunately, because the federal government canceled $11.4 billion in grants to local and state public health offices last month, the CDC is “scraping to find the resources and personnel needed to support Texas and other jurisdictions,” said David Sugerman, senior scientist for the agency’s measles response.
In addition to the US, Canada and Mexico are also battling measles outbreaks. Mexico’s outbreak has already been linked to the one in Texas, so the death of an unvaccinated adult in Mexico brings the total number of confirmed deaths in that outbreak to three (an additional adult in New Mexico was diagnosed with measles only after they died).
According to Your Local Epidemiologist, “Genetic sequencing shows Mexico’s outbreak (and thus, the Texas outbreak) is the same strain as Ontario’s outbreak (>600 cases), raising the likelihood that this one outbreak is now circulating across North America.”
The current larger outbreaks are shown below. The cases in Texas, New Mexico, Kansas, and Oklahoma all came from the same source; the outbreaks in Indiana, and Ohio are unrelated.
Monitoring skin that’s too painful to touch
Speaking of breath (see article above), did you know that your skin breathes, too? Researchers took advantage of this fact and developed a no-contact sensor that collects the gases the skin emits to develop a picture of the area’s health. It’s envisioned as being particularly useful for monitoring healing and diagnosing infection in open wounds.
Could overuse of CT scans raise cancer rates?
There was much buzz this week about a model-based study on the cancer risks that come with the use of computerized tomography (CT) scans. The study concluded that if clinicians continue to use CT scans at the current rate, and if the amount of radiation emitted by CT machines remains the same, “CT-associated cancers could eventually account for 5% of all new cancer diagnoses annually.” The analysis showed that the impact was largest on infants and children.
Why? CTs are basically a series of X-rays that are stitched together by a computer to create an image. X-rays are a type of ionizing radiation, which can cause cancer if someone is exposed to enough of it. While the study’s authors did not advocate rash action, one of their main concerns appeared to be overuse of CTs. “CT use is 30% higher today than in 2007,” they pointed out, “due to growth in low-value, potentially unnecessary imaging as well as population aging.”
The American College of Radiology has issued a rebuttal to this paper, saying, “There are no published studies directly linking CT scans (even multiple CT scans) to cancer.” They also pointed out that the “theoretical radiation risk proposed” by the study authors is “not based on actual patient outcomes.”
COMMENTARY: We see both sides of this discussion. Overexposure to ionizing radiation does carry risk. But how much and over what period of time is not clear today. In the meantime, keep track of your kids’ exposure to CT as well as your own, and discuss with your doctor if the next CT is truly necessary or not.
Where might a polygenic risk score fit in prostate-cancer screening?
Last June, we reported on a saliva-based test that rates an individual’s risk of getting prostate cancer, based on a group of genetic markers. Of the people in the highest-risk category (top 10%) in the study, 40% had prostate cancer, a much higher detection rate than the 25% that’s typical of the prostate-specific antigen test (PSA). And of those cancers, 55% were aggressive (PSA only detected 36% of these).
At the time, the test had just been presented at the annual conference of the American Society for Clinical Oncology. That research has now been published in the New England Journal of Medicine. An editorial accompanying the study noted that the test has been “validated only in men of European ancestry and performs less well among men of African and other ancestries.”
COMMENTARY: The editorial also asks the question, “Should a polygenic risk score be a first step in a screening pathway for an asymptomatic man who is worried about his risk of prostate cancer?” According to the author, the answer is not now, because we don’t yet have the infrastructure for it in the clinic. And if that infrastructure does arrive, he suggests that a better place for the test might be after a PSA, when such a test (once better validated for men of all ancestries) could be ordered for anyone with positive results.